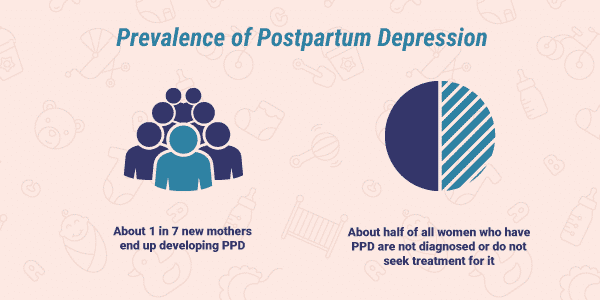
On this week's blog post, we are going to discuss postpartum depression (PPD). As women, there is often an increased feeling of pressure to excel and be the best at every task we are given and this includes being a mother. Not only mothers, but fathers too, can experience postpartum depression but put their feelings on the back burner leading to a delay in treatment. According to Postpartum Support International (2023), nearly 1 in 7 mothers and 1 in 10 fathers experience PPD. The first step in getting help is recognizing you are struggling with postpartum depression. Postpartum depression is sadness, increased irritability or anxiety, excessive worry, increased fatigue, decreased interest, or feeling overwhelmed that lasts for weeks to months following birth and impacts one's ability to perform daily life tasks (CDC, 2022).
Struggling with postpartum depression is nothing to be embarrassed or shameful of. In fact, many women struggle with it and fortunately, there are treatments available! Both psychotherapy and pharmacotherapy can be beneficial in recovering from postpartum depression. Common medications prescribed to a mother with PPD include selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, bupropion, and mirtazapine (Viguera, 2023). Each of these medications falls into the category of antidepressants and has been deemed not only safe for lactating mothers, but the benefits also outweigh the risks when taking them. Seeking care and getting better is important not only for the well-being of the parent but also for the infant and their development (Payne & Maguire, 2019). If you or someone you know is struggling with PPD, please seek help from your primary care provider or utilize the many resources available to you. You are not alone and there is light at the end of the tunnel.
Resources available to the public:
- Postpartum Support International: Provides helplines, support groups, and more!
- Office on Women’s Health: Provides quick answers to questions surrounding PPD and helps find areas to near you to get help.
- NAMI Minnesota: Provides a list of support groups and resources near you!
References
Centers for Disease Control and Prevention. (2022, May 23). Depression among women. Retrieved from https://www.cdc.gov/reproductivehealth/depression/index.htm#Postpartum
Payne, J. L., & Maguire, J. (2019). Pathophysiology mechanisms implicated in postpartum depression. Frontiers in Neuroendocrinology, 52(1), 165-180. https://doi.org/10.1016/j.yfrne.2018.12.001
Postpartum Suppor Internation. (2023). Get help. Retrieved from https://www.postpartum.net
Viguera, A. (2023, March). Mild to moderate postpartum unipolar major depression: treatment. UpToDate. Retrieved from https://www.uptodate.com/contents/mild-to-moderate-postpartum-unipolar-major-depression-treatment?search=postpartum%20depression&source=search_result&selectedTitle=2~146&usage_type=default&display_rank=2
I greatly appreciate the resources you provided for us on postpartum depression (PPD). I have friends that have reached out because they have noticed signs of PPD. I admire them for recognizing their symptoms and bravely reaching out for the help they needed. Dr. Langdon (2022) touches on guidance for partners, siblings, children, parents, in-laws, friends, and co-workers when supporting loved ones with PPD. I thought this could be super helpful because as you said PPD is nothing to be embarrassed or shameful of. Having a solid support group allows the individual affected by PPD feel accepted, understood, and validated (Langdon, 2023). PPD should not be the elephant in the room, it should be addressed straight on without any hesitation.
ReplyDeleteReferences
Langdon, K. (2022). Postpartum depression support. Postpartum Depression. https://www.postpartumdepression.org/support/
Langdon, K. (2023). Support group options for postpartum depression. Postpartum Depression. https://www.postpartumdepression.org/support/
Thank you for your post Tay. I really appreciate the resources that you provided and it is so important that moms and dad know about postpartum depression and understand it is not something to be ashamed off. Mayo (2022) states that the moms and dad who suffer from PPD are more likely to suffer from depression later in life. This is why this was such a good topic, because we need to start talking about PPD and make sure moms and dads know their resources. SSRIs are a great medication for PPD but there is lots of educations that needs to be done with this medication because of the rebound depression symptoms if stopped abruptly (Woo & Robinson, 2019). Let's keep this conversation going, its so important!
ReplyDeleteReferences:
Mayo Foundation for Medical Education and Research. (2022, November 24). Postpartum depression. Mayo Clinic. Retrieved April 13, 2023, from https://www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617
Moser Woo, T, and Robinson, M. (2019). Pharmacotherapeutics for Advanced Practice Nurse Prescribers (5th). F.A. Davis Company. ISBN-13: 978-0-8036-6926-0